
Separating Fact from Fiction: The Truth About Anti-Aging Supplements
Are you on the hunt for the secret to staying …
Separating Fact from Fiction: The Truth About Anti-Aging Supplements Read MoreLet's Talk Total Health

Are you on the hunt for the secret to staying …
Separating Fact from Fiction: The Truth About Anti-Aging Supplements Read More
Hey there! Let’s talk about something super important for both …
Why You Should Get Your Testosterone Levels Checked? Read More
When someone you care about is going through the challenging …
Embracing the Role of Support in Recovery Read More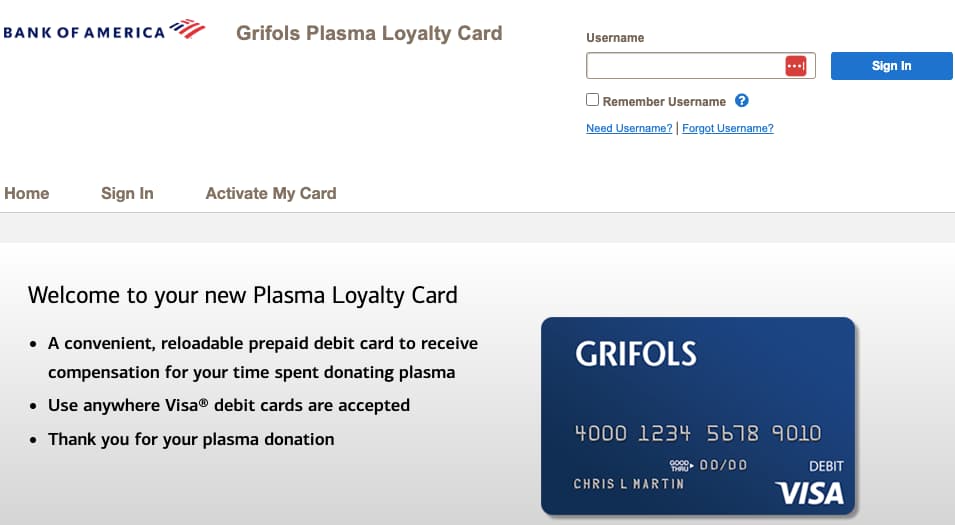
Hey there! Today, we’re going to talk about something cool …
Bank of America Plasma Loyalty Card Activate Login Account Read More
Alcohol addiction is a pervasive problem that requires attention to …
Best Alcohol Addiction Treatment Options in 2024 Read More
Hey there fitness enthusiasts! Are you looking to pack on …
Best Bodybuilding Supplements for Muscle Mass in 2024 Read More
Movement is not only a form of physical activity but …
The Joy of Movement: 8 Hobbies for Dancers and Gymnasts Read More
Regardless of the industry a worker is operating in, an …
Should Reducing Medical Care Professional’s Workloads be the Key Goal of Healthcare Organisations in 2024? Read More
Hey there fitness enthusiasts! Are you curious about joining the …
Lifetime Membership Cost 2024 Near Me Prices Read More
You must be logged in to post a comment.